Skincare Tips
Winter is underway, and the drop in temperature is here to remind you! By now, you may be tackling tight or dry skin, chapped lips rough knuckles and itchy scalps. It’s official… Winter can certainly wreak havoc on your skin’s health!
These skin care woes might be the bane of your existence during this chilly time, so we have asked renowned dermatologist, Dr Christopher Dobson for top tips on keeping blustery conditions from bothering your skin.
What Happens to Your Skin in the Winter?
Winter is not only known for introducing new skin issues, but it’s famous for causing flare-ups in those already living with certain skin conditions.
This is in part due to Filaggrin, one of the most important proteins in our skin for maintaining the barrier function and natural moisturizing factors.
During the winter, the levels of Filaggrin decrease, and when this is combined with the dry cold weather, low humidity, and indoor heating that dehydrates our skin, it leads to an unhappy complexion and the worsening of skin conditions for many people.
Here are five common winter skin issues that may worsen during the wintertime.

Eczema
Eczema is a common skin condition. The most common form, atopic eczema, affects 1 in 5 children and 1 in 10 adults in the UK. Characterized by inflamed, red, itchy patches of skin, eczema is caused by a combination of immune system activation, environmental triggers, and stress. Cold dry weather can trigger eczema flares in winter.
Psoriasis
Psoriasis is a long-term autoimmune skin disease that causes red, itchy scaly patches on the skin, which flare up for a few weeks or months before subsiding or going into remission. The most common sites for psoriasis are your knees, elbows, trunk, and scalp. Cold weather and decreased sunlight can cause worsening psoriasis in the winter.
Rosacea
Rosacea is a common skin condition causing blushing or flushing in your face and eyes. Rosacea may flare up for weeks or months before subsiding or going into remission. If left untreated, rosacea can lead to permanent damage to the skin and eyes. Cold weather is a common trigger for many.
Chilblains
Chilblains are the painful inflammation of small blood vessels in your skin that occur in response to repeated exposure to cold air. Symptoms include itching, red patches, swelling and blistering on your hands and feet.
Windburn
Windburn is a common problem in winter. Caused by cold temperatures and wintry air which sucks the moisture out of our skin. This causes blood vessels near the surface to expand, which reddens the skin in much the same way that sunburn does.

Importance of Winter Skin Care
During the winter, skin tends to lose moisture and oil due to a lack of humidity in the air, harsh weather and of course, central heating.
These conditions cause dryness and dehydration which in turn, may lead the skin to become dry, itchy, flaky tight or sensitive.
If you’re noticing some of these symptoms, we recommend changing your skincare routine during the colder month to keep your skin happy, healthy and hydrated.
Winter weather is certainly tough on your skin, but these top ten tips from Dr Dobson should get you through the rest of the season!
Moisturize Frequently
When it comes to looking after dry, itchy winter skin, it’s all about moisture. This one might seem obvious, but moisturizing your skin is crucial for keeping it hydrated throughout the winter.
A thicker and richer moisturizer can be used to replace as much as possible of that lost water and help to lock it into the skin.
Moisturizing just after washing is not only comforting but helps add a protective layer to keep your skin looking smooth and hydrated, reducing the appearance of blemishes, while plumping up fine lines and wrinkles.
For winter, use a gentle moisturizer at least twice a day after cleansing- in the morning and before bed at night to keep your skin soft and supple.
Switch to Hydrating Cleansers
During the winter months, avoid harsh cleansers on the face. We want to make sure a gentle cleanser is being used, something nice and hydrating.
As a rule of thumb, any cleanser that leaves you ‘squeaky clean,’ is stripping the skin of natural moisture.
Anything that is relatively aggressive – maybe it has a high salicylic acid content – is going to cause further moisture loss and irritated skin. Switch to gentle, hydrating, fragrance-free cleansers for daily cleansing and to remove makeup.
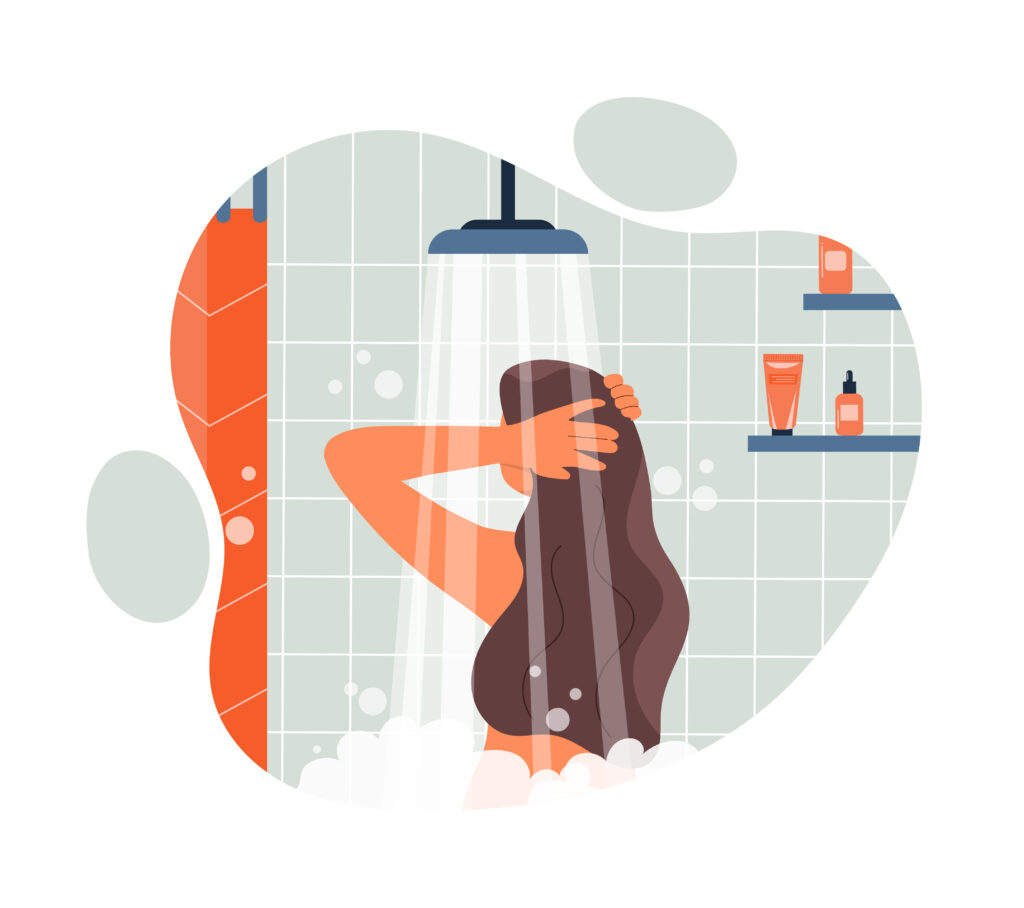
Limit Hot Showers
Winter weather brings the desire for long hot showers, but hot water will only further dry out your skin.
When it comes to dry, itchy skin on the body, one of the quickest changes you can make is lowering the temperature in the shower, as well as limiting the duration.
Limit showers to 15 minutes and use lukewarm water to avoid irritating your skin.
Avoid Harsh Scrubs and Scented Products
Your skin is dealing with unusually high levels of inflammation so try not to beat it up any further with a physical exfoliator. Loofahs, bath mitts, and gritty scrubs can irritate dry skin and lead to eczema flares. Avoid these if you have a history of eczema or dry skin. Instead, switch to using unscented soaps and body washes.
Exfoliate for Smooth, Supple Skin
Dry skin will stay dry without light exfoliation. Using a good quality exfoliator can remove the damaged top layer of the skin and help facilitate new skin cell growth.
Try to avoid using soaps as these contain a high PH, which can lead to more dryness and oftentimes inflammation.
Also, if possible, avoid rubbing your skin with a towel as this can exacerbate the problem. Instead, gently blot your skin to dry off.

You Still Need Sunscreen!
Just because it is winter, it doesn’t mean you should put away your suncream.
Even though the sun’s UVB rays are not as strong in the winter, levels of UVA (or UV-Ageing as it is known in the dermatology world) are still significant enough to age your skin.
Not to mention, the reflection of the sun’s rays through the clouds and off the snow can cause you to get serious sunburn even if it’s not sunny outside.
Remember to wear SPF 30+ that specifically has a high UVA rating, every morning and reapply if doing any outdoor winter activities.
Carry Lip Balm
Help keep dry lips from getting chapped and sunburned during winter by using a hydrating lip balm every morning and throughout the day to seal in moisture. It moisturizes your lips, so they stay hydrated ensuring that they’re protected from the elements. Plus, many lip balms contain sunscreen, which is just as important during the winter as it is during the summer.
Be Aware of Irritating Skincare Products
As we spend more time indoors during the colder months, it’s easy to become complacent or even lazy when it comes to taking care of your skin.
Make the effort to be faithful to a daily skincare routine. Use a gentle cleanser to help remove irritants followed by your favourite serum and a heavy moisturizer.
If you’re unsure which routine is right for you, make an appointment with our skin specialist for guidance. Be aware of using potentially irritating ingredients such as retinoids, exfoliating acids, and vitamin C.
You may need to dial back on the potency of these to be able to use them consistently through winter without causing excess irritation.

Keep Hydrated
Staying adequately hydrated is just as important during the winter as it is in the summer. Staying hydrated by drinking plenty of fluids is one of the best things you can do via your diet to avoid dryness. A few healthy ways to increase your daily water intake include:
- Carry a refillable water bottle with you
- Add a squeeze of fresh fruit to your water for flavour variety
- Make water your drink of choice for meals and snack times
- Avoid sugary beverages such as coke or energy drinks
- Try making half of your plate fruits and vegetables, which is an easy way to incorporate extra fluid at mealtimes.
With these tips, you can be successful in your efforts to stay hydrated and healthy throughout the winter months.
Give Your Face a Massage
One of the most powerful steps in a winter skincare regimen is a facial massage, which reduces fluid build-up and in turn sculpts the face. When it comes to your moisturiser, take time to massage it into your skin. Try for at least 30 seconds to maximise its effects – it’ll help with absorption and circulation. When you boost blood flow, the haemoglobin will be carry more oxygen to the tissue and brighten the skin.

Get checked
Overall, the best tip we can give you is to schedule a regular annual check-up with a dermatologist especially if dry, irritated skin doesn’t heal or gets worse.
It’s very important to diagnose, treat and rule out an underlying medical condition like an allergy, dermatitis, or something more severe.
Our dermatology team are here to are here to help you!
They can analyse your skin type, troubleshoot your current skin care regimen, and give you advice on the skin care products you should be using. They can also provide medication to address specific skin concerns when over-the-counter products aren’t working.
A visit to a dermatologist is also vital if you notice any concerning changes in your skin, such as the size of a mole or new persistent rash. Dr Dobson is a highly respected and vastly experienced consultant. He is a part of our outstanding team as a Consultant Dermatologist providing personalised care, diagnosis and treatment of skin conditions.
Get in contact
To book your consultation, call our team on 01772 663977 or if you prefer to email us on [email protected].