Endometriosis: what it is and when should you seek treatment
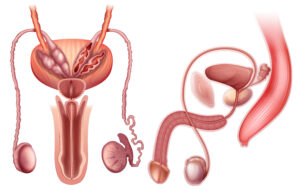
Endometriosis is a disease in which tissue similar to the endometrium (the tissue that lines the inside of the uterus or womb) is present outside of the uterus. Endometriosis most commonly occurs in the lower abdomen or pelvis, but it can appear anywhere in the body. It may spread to the ovaries, fallopian tubes, uterus, bowel or bladder, or anywhere inside the abdominal cavity.
Often, endometriosis causes pain far greater than would be expected during a normal menstrual cycle, but even in cases where no pain is experienced, the condition can lead to organ damage, internal scarring and infertility.
Key facts
- Endometriosis affects roughly 10% of reproductive age women and girls globally.
- It is a chronic disease associated with severe, life-impacting pain during periods, sexual intercourse, bowel movements and/or urination, chronic pelvic pain, abdominal bloating, nausea, fatigue, and sometimes depression and infertility.
- Endometriosis can start at a person’s first menstrual period and last until menopause.
- There is currently no known cure for endometriosis and treatment is usually aimed at controlling symptoms.
- Access to early diagnosis and effective treatment of endometriosis is important, but is limited in many settings, including in low- and middle-income countries.
What are The Symptoms of Endometriosis?
Some of the symptoms of endometriosis may at first seem to overlap with normal symptoms that occur during the menstrual cycle. This is because menstruation affects women differently; some experience longer periods or heavier bleeding, some experience bloating or lower back pain while others do not. This means it is important to be aware of what is normal for you, so you can more easily identify when things feel different.
Pain is the most common symptom of endometriosis. Women with endometriosis can experience pelvic or lower abdominal pain, pain with intercourse and pain during bowel movements. Symptoms can be constant or “cyclical,” meaning that they worsen before and during the period, and then improve. Women may have constant pelvic or lower abdominal pain as well. Other symptoms include infertility, bowel and bladder symptoms (bloating, constipation, blood in the urine, or pain with urination), and possibly abnormal vaginal bleeding.
Common Symptoms
- Period pain that prevents you from following your normal routines
- A cramping or stabbing pain in your pelvis that gets worse during your period
- Lower back pain or lower tummy pain that gets worse during your period
- Pain during or after sex
- Difficulty getting pregnant
- Excessively heavy periods
Of these symptoms, excessively heavy periods is often one of the hardest to judge. While every woman’s menstrual cycle differs slightly, there is some general guidance on what is normal.
What is ‘normal’ for a period
It’s hard to say what’s normal, as every woman has a menstrual cycle that is unique to her. On average, a cycle lasts 28 days, but a normal menstrual cycle could be as short as 22 days or as long as 36 days.
Your period can last between 2 and 7 days, but it will usually last for about 5 days. The bleeding tends to be heaviest in the first 2 days. When your period is at its heaviest, the blood will be red. On lighter days, it may be pink or brown. You’ll lose about 20 to 90ml (about 1 to 5 tablespoons) of blood during your period, although some women bleed more heavily than this.
Some women experience PMS (premenstrual syndrome) as part of their menstrual cycle, which includes symptoms such as breast tenderness, headaches, mood swings, tiredness, bloating and changes in sex drive and appetite. PMS usually goes away once a period starts.
You may be experiencing a heavier than ‘normal’ period if you’re:
- bleeding through your clothes
- passing large clots
- having to change your period product more frequently
- having to use 2 different products at the same time
- having heavy periods every month that stop you doing everyday activities
Untreated heavy or prolonged bleeding can stop you from living your life to the fullest. It also can cause anemia. Anemia is a common blood problem that can leave you feeling tired or weak.
Do heavy periods mean you have endometriosis?
Not in all cases. Heavy, painful menstrual bleeding does not mean there is anything seriously wrong but could be a sign of fibroids, endometrial polyps or endometriosis. In post-menopausal women, vaginal bleeding can also be a sign of cancer of the womb. According to the NHS, the cause of heavy periods is unknown in about half of women.
Treatment for heavy periods
Depending on how heavy your periods are, there are several treatment options available. Heavy periods do not always need to be treated. But there are treatments that can help if they’re affecting your daily life.
Treatments from a GP include:
- some types of contraception, such as an intrauterine system (IUS) or the combined contraceptive pill
- medicine to help reduce the bleeding, such as tranexamic acid
- prescription-only anti-inflammatory painkillers, such as mefenamic acid or naproxen
If these treatments are not successful, there are also surgical options. The one you are recommended will depend on various factors personal to you, including your age and whether you have completed your family, as well as the cause and severity of your symptoms.
In this procedure a laser or heat is used to destroy the lining of the uterus resulting in lighter periods.
- Focused ultrasound surgery
This is a non-invasive procedure where ultrasound waves are used to destroy fibroid tissue and shrink fibroids.
This is the removal of your cervix and uterus. It results in the permanent end of your periods and stops you from being able to get pregnant. If you have your ovaries removed at the same time this will trigger immediate menopause.
When should you visit a doctor?
You know your body and your menstrual cycle better than anyone else. If you are worried about how much you are bleeding during your menstrual cycle, have noticed your periods have become heavier or are experiencing some of the other common endometriosis symptoms, such as severe period pain, then it is time to schedule an appointment with your doctor.
Investigating your symptoms
At Greater Lancashire Hospital, we have some of the UK’s leading experienced consultants specialising in women’s health, who can thoroughly investigate your symptoms and offer a treatment plan to resolve or reduce them.
Diagnosis of heavy periods starts with a set of questions that include other symptoms, your current medical conditions, medicines that are being taken followed by physical examination of your abdomen and pelvis. This can help them detect the presence of fibroids. They may also recommend an ultrasound scan, which uses high-frequency sound waves to create images of the tissues within your body. This can help detect a range of conditions, including fibroids, endometriosis and cancer.
If the results of these tests and examinations are unclear and depending on your symptoms and medical history, you may be referred to for further tests, such as a laparoscopy. This is a type of keyhole surgery where a small incision is made into the abdomen so that a thin tube can be passed through. This tube has a light and a camera at the end of it which allows your consultant to detect the presence of any excess tissue growth caused by endometriosis.
Treating endometriosis
If you are diagnosed with endometriosis, there are several treatment options available to reduce your symptoms. Your doctor will advise you on which are best depending on how severe your symptoms are and your medical history. No treatments cure the disease.
Your gynaecologist will discuss the treatment options with you and outline the risks and benefits of each.
Anti-inflammatories such as ibuprofen or paracetamol, may be tried to see if they help reduce your pain. They can be used together for more severe pain.
The aim of hormone treatment is to limit or stop the production of oestrogen in your body, as oestrogen encourages endometriosis tissue to grow and shed. One of the main hormone-based treatments for endometriosis includes the combined oral contraceptive pill.
Surgery can be used to remove or destroy areas of endometriosis tissue, which can help improve symptoms. The kind of surgery you have will depend on where the endometriosis is and how much of it there is. Some of the options are: Laparoscopy, the most commonly used technique, where small cuts (incisions) are made in your tummy so the endometriosis tissue can be destroyed or cut out.
Alternatively, If keyhole surgery and other treatments have not worked and you do not want to try to get pregnant, removal of the womb (a hysterectomy) might be an option. A hysterectomy is a major operation that will have a significant impact on your body.
Getting Help
You are not alone with your symptoms. Endometriosis is a common condition affecting one in 10 women. Early diagnosis can help with treatment. If you are concerned, don’t suffer in silence. Book a consultation with our kind and discreet gynaecological experts. You can call us on 01772 663977, email the team on info@greaterlancashirehospital or send us a secure message on our website.